Salmonella Bacteria
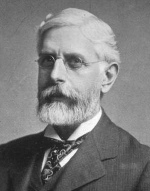
Named after American veterinary pathologist, Daniel Salmon (
at right, 1850-1914), but actually discovered by his assistant, Theobald Smith, a subspecies of
Salmonella isolated from pigs was first described by both men in 1885.
Salmonella bacteria (sounds better than 'Smithella' don't you think?) fall into one of two large species groupings: either S. bongori or S. enterica.
Within those two species, there are over 2000 known 'serovars' (a fancy name for subspecies),
all sharing 95% or more of the same DNA. Most bacteria mutate fairly easily, which might explain why this genus has such an extended family. In fact, Salmonella is related to E. coli, and shares 60-70% identical DNA with it.
Although Salmonella bacteria are found almost everywhere, many are specific to one organism. One of the more notorious, the strain responsible for typhoid fever, S. typhi, is found only in humans. In cattle, three serovars are typically found: Salmonella dublin, S. typhimurium and S. newport, the first two being the most common.
Usually, if everything is functioning well in the cow's rumen (stomach), exposure to volatile fatty acids (VFAs) produced by the normal microbial flora there will kill Salmonella. When things get out of whack with the cow's diet (too much brewer's grain, for instance) conditions will actually favor its growth. In order to keep the cows healthy, farmers will often give the infected animals an antibiotic.
Those cells not killed by the drug then multiply (a bacteria's generation or doubling rate can be as little as 20 minutes) and soon the cow is sick again.
Already, a new serovar of S. typhimurium, designated DT 104 has developed resistance to the antibiotics ampicillin, chloramphenicol, streptomycin, the sulfonamides and tetracycline.
Sadly, overuse of antibiotics by dairy farmers, forced to dose their cows because the feed is sickening them, has been a major source of drug resistant bacteria in recent years.

As luck would have it, S. typhimurium (at right, invading cultured human cells. Courtesy, Rocky Mountain Labs, NIAID, NIH) is also one of the most common causes of food poisoning in humans.
Though rarely fatal, the abdominal cramps, nausea, vomiting and diarrhea (along with occasional fever and chills) can last for up to seven very unpleasant days. The main pathway to infection is usually consumption of food contaminated with feces, but dirty hands work just as well.
Raw milk from cows fed a high-percentage green grass diet (preferably organic) has all of its antibiotic defense systems fully functional. As mentioned earlier, should the cow ingest something contaminated with Salmonella, the VFA's in her rumen will do such a good job of eradicating it that her manure will likely be pathogen-free as well.
Should something she laid on in the pasture somehow get into her milk, there's lactoferrin, lysozyme, lactoperoxidase, numerous immunoglobulins and, of course, lactic acid, all waiting to take action against the doomed bacteria. Clean, raw milk is a living food, fully capable of defending itself, as it's successfully done for millennia.